Diagnosing Melanoma Correctly
Most melanoma diagnoses begin with the patient, a loved one, or a doctor noticing a new, abnormal, or changing mole or lesion on the skin. As with many kinds of cancer, early detection and treatment is critical to preventing early stage melanoma from progressing to the more advanced stages. Knowing the ABCDEs of melanoma identification and performing regular self-checks and check‐ups are crucial steps in treatment and prevention. Before an official melanoma diagnosis can be made, however, your doctor will biopsy the lesion and send it to a pathologist who will look at it underneath a microscope to confirm the diagnosis.
Below is a list of the types of biopsies typically done on lesions suspicious for melanoma.
- Shave Biopsy: In a shave biopsy, a scalpel or blade is used to remove a thin layer of tissue off of the suspected site. A shave biopsy does not penetrate below the dermis, and results in minimal scarring.
- Excisional Biopsy: In an excisional (or incisional) biopsy, a larger piece of tissue is cut away. Compared to a punch biopsy, an excisional biopsy will likely be used when the suspected tumor has grown thicker or deeper into the tissue. In many cases, an excisional biopsy will be used to completely remove the suspicious area. If the biopsied lesion is found to be cancerous, but no additional cancerous cells are found at the site, treatment may be effectively complete.
- Punch Biopsy: After applying a topical anesthetic the physician uses a small round tool to cut away the piece of skin being sent to biopsy.
Once the suspected lesion is viewed under the microscope and confirmed to be cancerous, the doctor will proceed by staging the tumor. Cancer staging is the process of determining how much cancer is in the body and where it is located. Staging describes the severity of an individual's cancer based on the magnitude of the original tumor as well as the extent the cancer has spread in the body. Learn more about how melanoma is staged here.
Treatment Options and Strategies
Depending on the particular stage of your melanoma diagnosis, there may be several treatment options available to you. Because each case is unique, your doctor will want to review your full pathology report and medical history when discussing treatment in order to determine the best course of action. If you have been recently diagnosed with
melanoma, learning about treatment options is of the utmost importance. There are many centers around the United States that specialize in diagnosing and treating melanoma.
Not sure where to go? Visit the Melanoma Research Foundation’s Treatment Center Finder or take advantage of our Find a Dermatologist page to help find the right place for you.
Types of Treatment:
These are examples of the types of treatment available for melanoma. Based on your personal history, pathology report, and stage at diagnosis, your doctor may recommend one or more of the following:
- Surgery
- Clinical Trials
- Immunotherapy
- Targeted Therapy
- Chemotherapy
- Prognosis
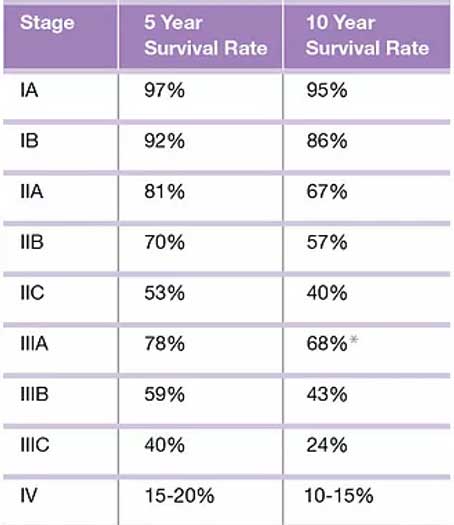
Survival rates tell you what portion of people with the same type and stage of cancer are still alive a certain amount of time (usually 5 or 10 years) after they were diagnosed. The survival rate is the percentage of people who live at least a certain amount of time after being diagnosed with cancer. For example, the 5-year survival rate for Stage IIA melanoma is around 81%, this means that about 81% of patients with this tumor stage survive 5 year or longer after their initial diagnosis.
Survival rates do not always tell the whole story as they are often based on previous outcomes of large number of people who had the disease, but every patients’ case is different. It’s important to remember that survival rates are based on the cancer stage when it was first diagnosed, and not ones that have returned. They can’t tell you how long you will live, but they may help give you a better understanding about how likely it is that your treatment will be
successful. Some people will want to know the survival rates for their cancer, and some people won’t. If you don’t want to know, you don’t have to.
The above survival rate tables are based on nearly 60,000 patients who were part of the 2008 American Joint Committee on Cancer (AJCC) Melanoma Staging Database.
Side Effect Management
Every type of cancer treatment can cause side effects or modifications to your body and how you feel. For diverse reasons, individuals do not always experience similar side effects even when they are given the same treatment for the same type of cancer. This makes it difficult to predict how you will feel during treatment. The
more that newly diagnosed melanoma patients know about how to manage their care and its side effects, the better they will feel in the long run.
In partnership with leading melanoma oncology experts, The AIM at Melanoma Foundation has developed comprehensive and up-to-date information on all aspects of every melanoma treatment currently approved by the U.S. Food and Drug Administration. Click Here to view the list.
Life After Melanoma
For most people, the cancer experience doesn't end on the last day of treatment. Life after cancer brings challenges that can last a lifetime and many melanoma survivors find it hard not to worry about cancer growing or coming back.
Follow-up After Melanoma
After treatment, your doctors will still want to monitor your skin closely. In addition to risk of melanoma coming back, people who have had melanoma have a higher risk of developing another one. This is why it is important to keep all follow-up appointments. During these appointments, your doctors will ask about any problems you may be experiencing and might perform exams and lab or imaging tests to look for signs of cancer or treatment side effects.
Some treatment side effects may last a long time or might not even show up until years after your treatment has been completed. Follow-up appointments are also a good time to ask questions and talk about any changes or problems you notice or concerns you might have.